From Blueprint to Business: AI Surgical Video Summarization
Designing and launching a hybrid physical-digital service for surgical video management
Results
Delivered an AI-driven service that shortens surgical videos for multiple contexts including clinical trials, ENT procedures, and conferences.
Reduced review times for clinicians and researchers by targeting only relevant video segments.
Created a scalable service blueprint that integrates with existing OR workflows and compliance systems.
Enabled potential storage cost reductions of more than 60 percent through summary-first archival.
Context and Vision
Surgical videos are critical for clinical research, training, and peer collaboration. They are also long, storage-heavy, and hard to navigate. In our HCDE master’s capstone, our team (Chronicle) investigated how to make these videos more useful without adding friction to already complex surgical workflows.
Our vision was to create a service that would deliver concise, context-relevant summaries without compromising compliance or clinical detail. The capstone ended with a validated service blueprint and MVP concept. Immediately after graduation, my teammate Jack and I spun the idea into a startup called Brevity AI, expanding the concept into a full-fledged physical-digital service.
Part 1: Chronicle – Discovery and Blueprinting
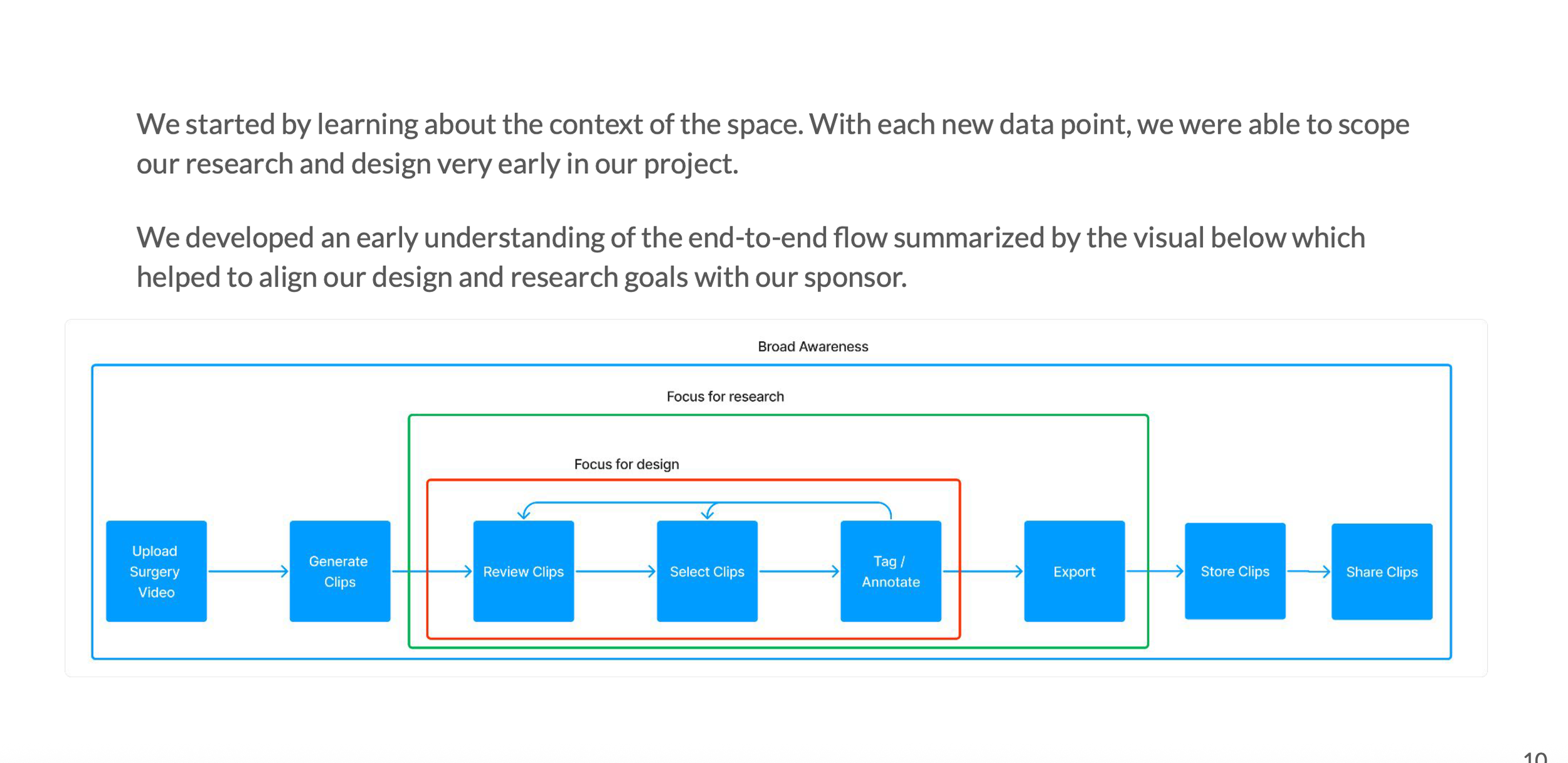
Understanding the Current Workflow
Our first step was to map the journey of surgical videos from capture to review. We documented both physical and digital touchpoints, including how videos were retrieved from the surgical tower, uploaded to secure storage, and later accessed for clinical or educational purposes.
Artifact: Workflow diagram
Caption: Early mapping of the surgical video lifecycle, from in-OR capture to secure storage and review.
Research Approach
We combined secondary research, contextual inquiries, and in-depth interviews with surgeons, an AI developer, and a clinical trial coordinator. This gave us insight into both the frontstage experience (surgeon interaction with tools and systems) and the backstage dependencies (hospital IT systems, storage processes).
Artifact: Research methods overview

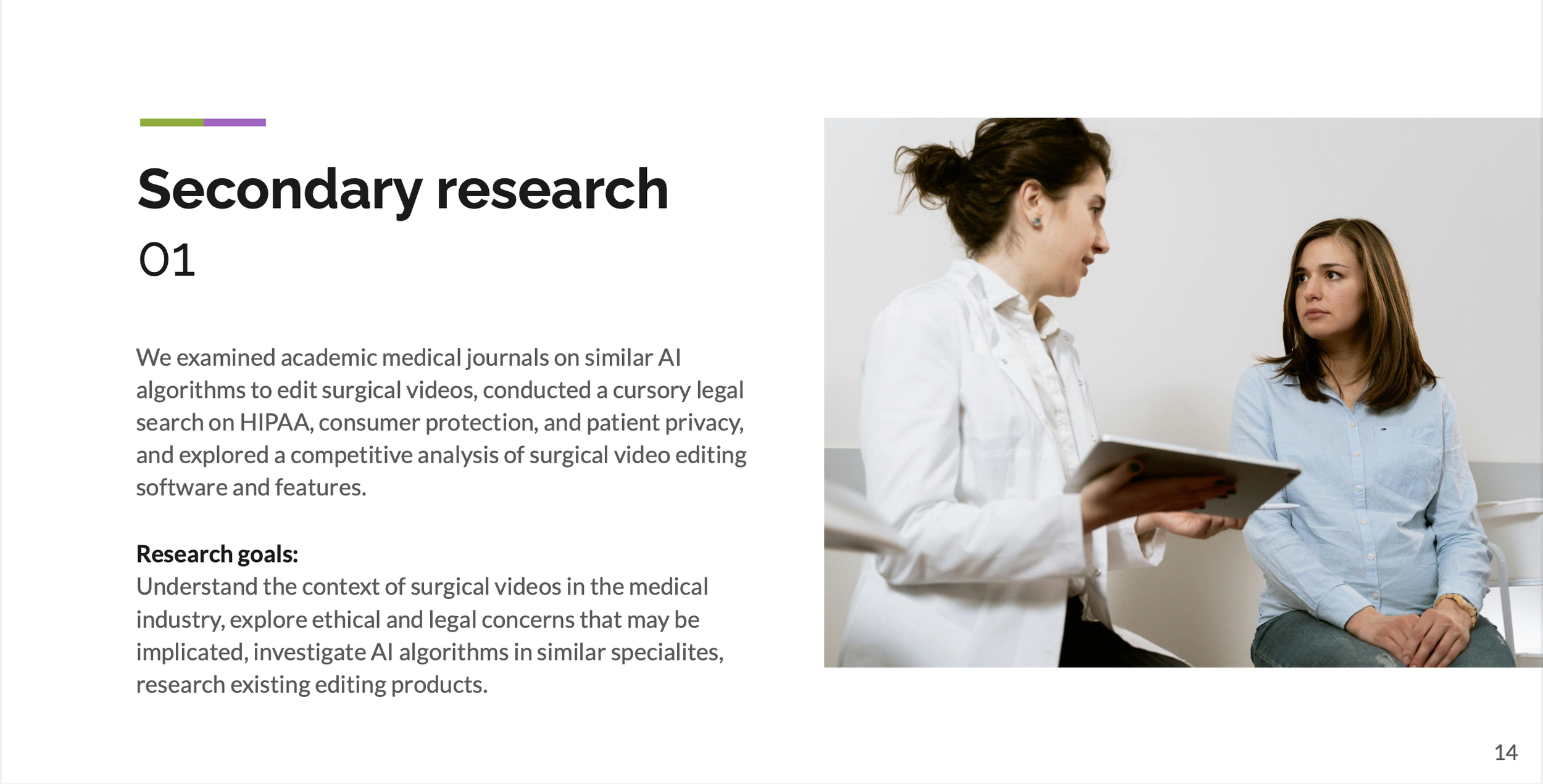
Caption: Multi-method research plan integrating observational studies, interviews, and literature review.
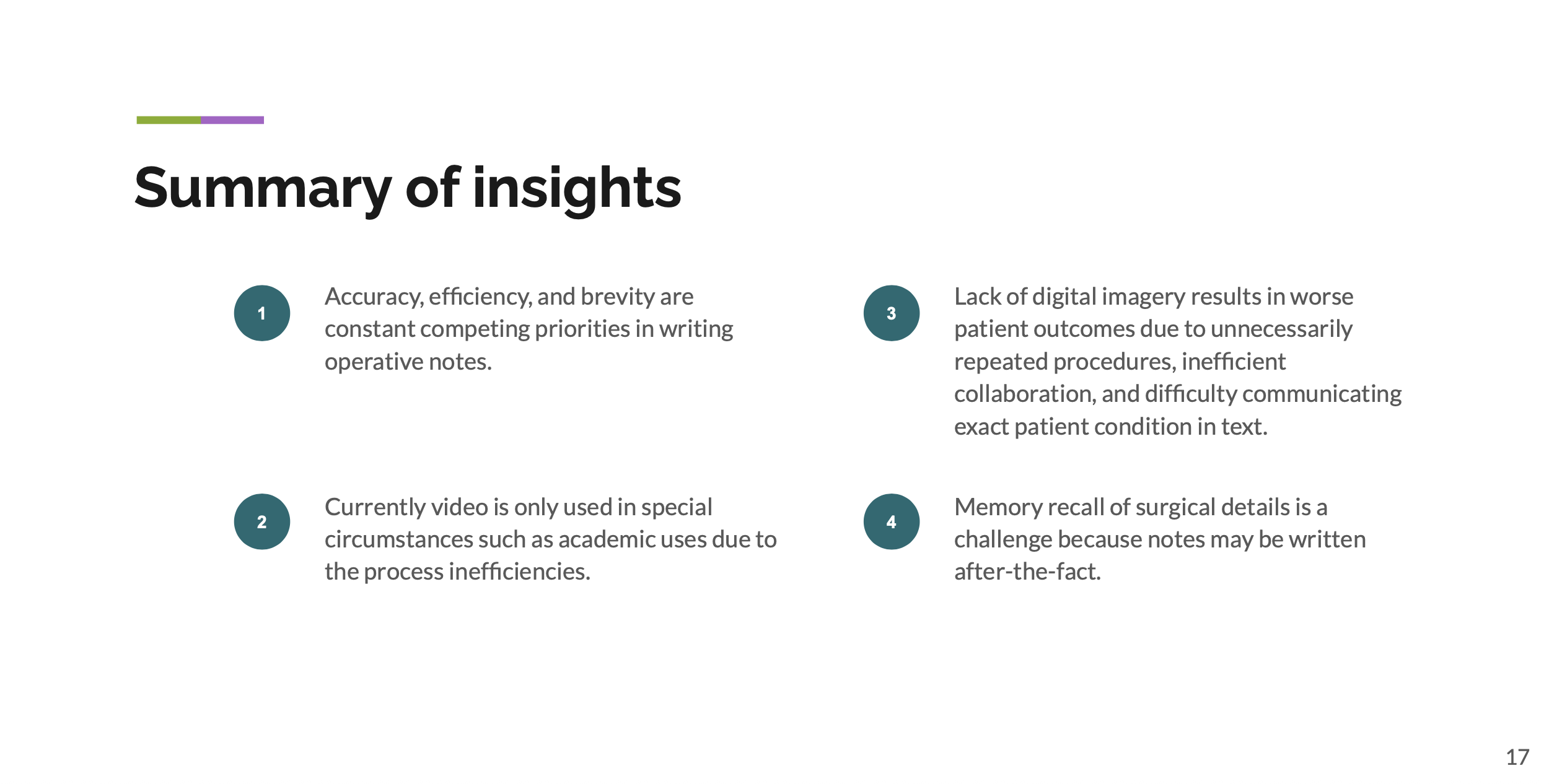
Key Insights
We identified recurring pain points:
Inefficient review processes due to long, non-indexed footage.
Under-usage of stored videos because of retrieval complexity.
Risk of compliance breaches when sharing raw footage.
Artifact: Insights summary table
Caption: Pain points aligned to opportunities for intervention at specific touchpoints.
Mapping the Ecosystem
We mapped the ecosystem by creating a detailed user flow that captured every step in the surgical video process, from in-OR capture to post-surgery review and sharing. This helped us visualize where different users such as ENT residents, attending surgeons, and support staff would engage with the system.
From there, we developed early sketches and storyboards to illustrate how the service would fit into real surgical and post-operative workflows. These artifacts gave us a clear picture of how the physical and digital components needed to connect, and where the main opportunities for intervention were.
Artifact: Sketching and storyboards, user flow




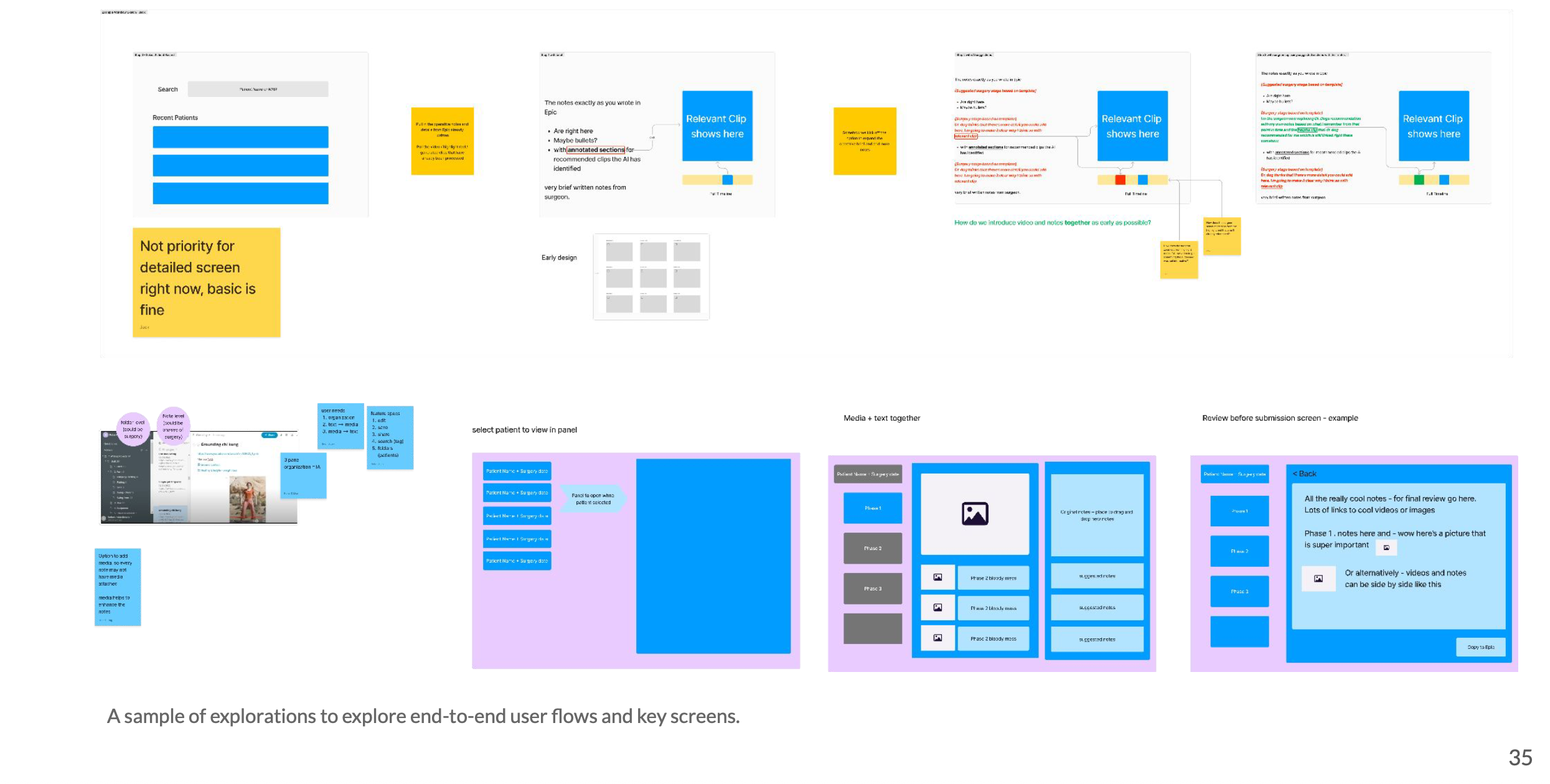


Caption: Visual exploration of interactions and service touchpoints for the surgical video workflow.
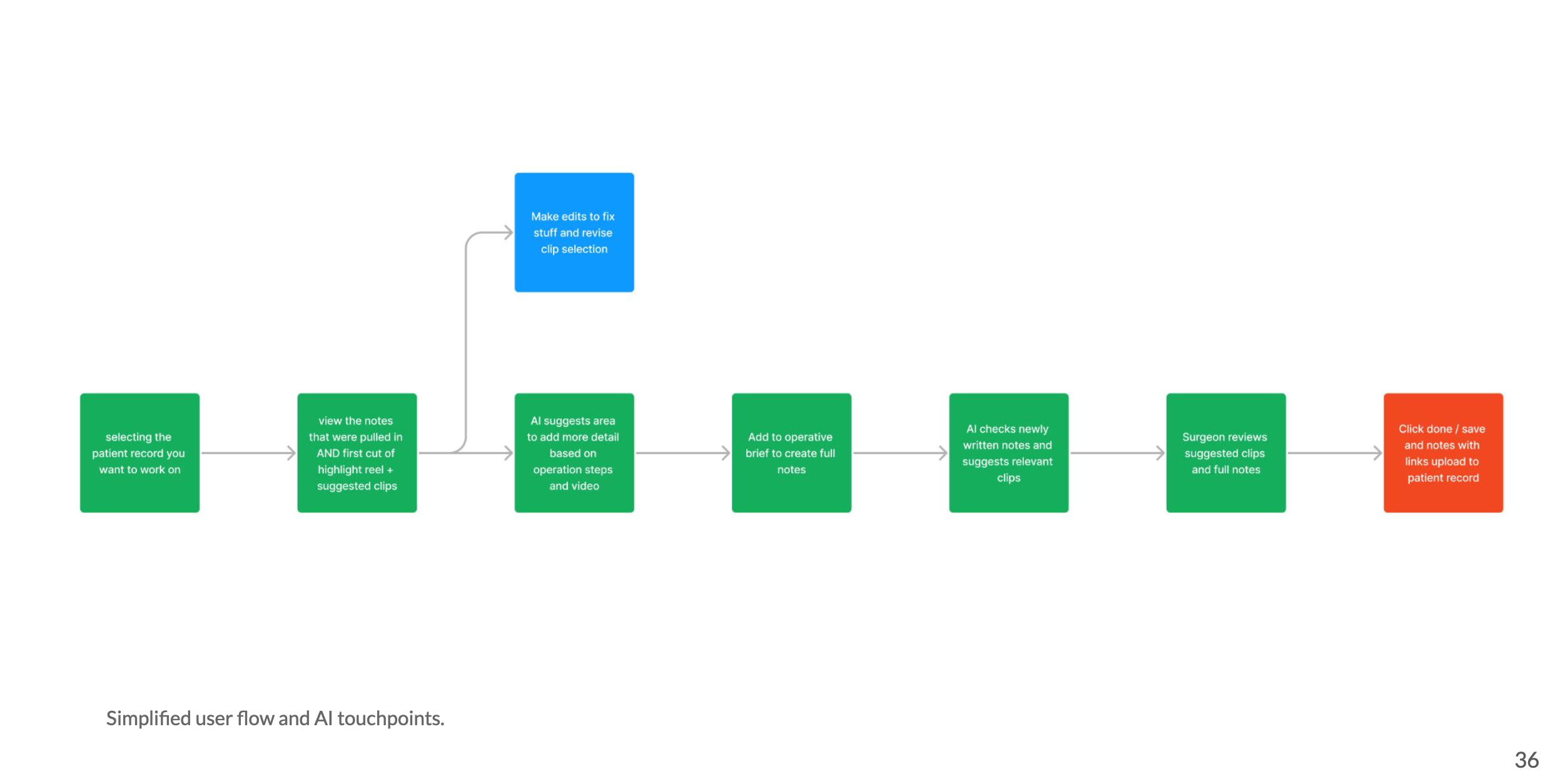
Defining the Concept and Final Design
The synthesis of feedback from sketching, storyboarding, and user flow explorations led to alignment on a core set of 13 user interactions that became the foundation for our design work. These interactions, documented below, reflected the most critical actions users needed to take within the tool.
Artifact: User interactions list
Caption: Agreed set of 13 priority interactions guiding the design direction.
From there, we developed wireframes to establish the basic structure and layout of each key screen. These appear below and gave us a shared visual language for stakeholder discussions.
Artifact: Wireframes


Caption: Early structural layouts exploring arrangement of navigation, video playback, and annotation features.
We then moved through multiple rounds of design iterations, refining functionality and visual hierarchy. The designs below show this progression, from mid-fidelity layouts to more refined compositions, including feedback incorporated from peers, instructors, and our sponsor.
Artifact: Design iterations




Caption: Progressive refinement of the UI through mid- and high-fidelity prototypes.
To validate these changes, we conducted evaluative testing with both peers and our sponsor. The artifacts below capture this stage, highlighting observations, feedback, and adjustments made to improve usability and alignment with surgeon workflows.
Artifact: Evaluative testing sessions

Caption: Testing with sponsor to refine interaction flow and visual clarity.
Chronicle – Closing and Transition
This process culminated in a set of key screen flows that included the landing page, review bookmarks, search, and publish views, as well as a diagram for visually distinguishing AI-suggested, manually created, and bookmarked clips. Accessibility considerations were integrated before delivery of the final high-fidelity designs.
Artifact: Key screen flows and final high-fidelity designs



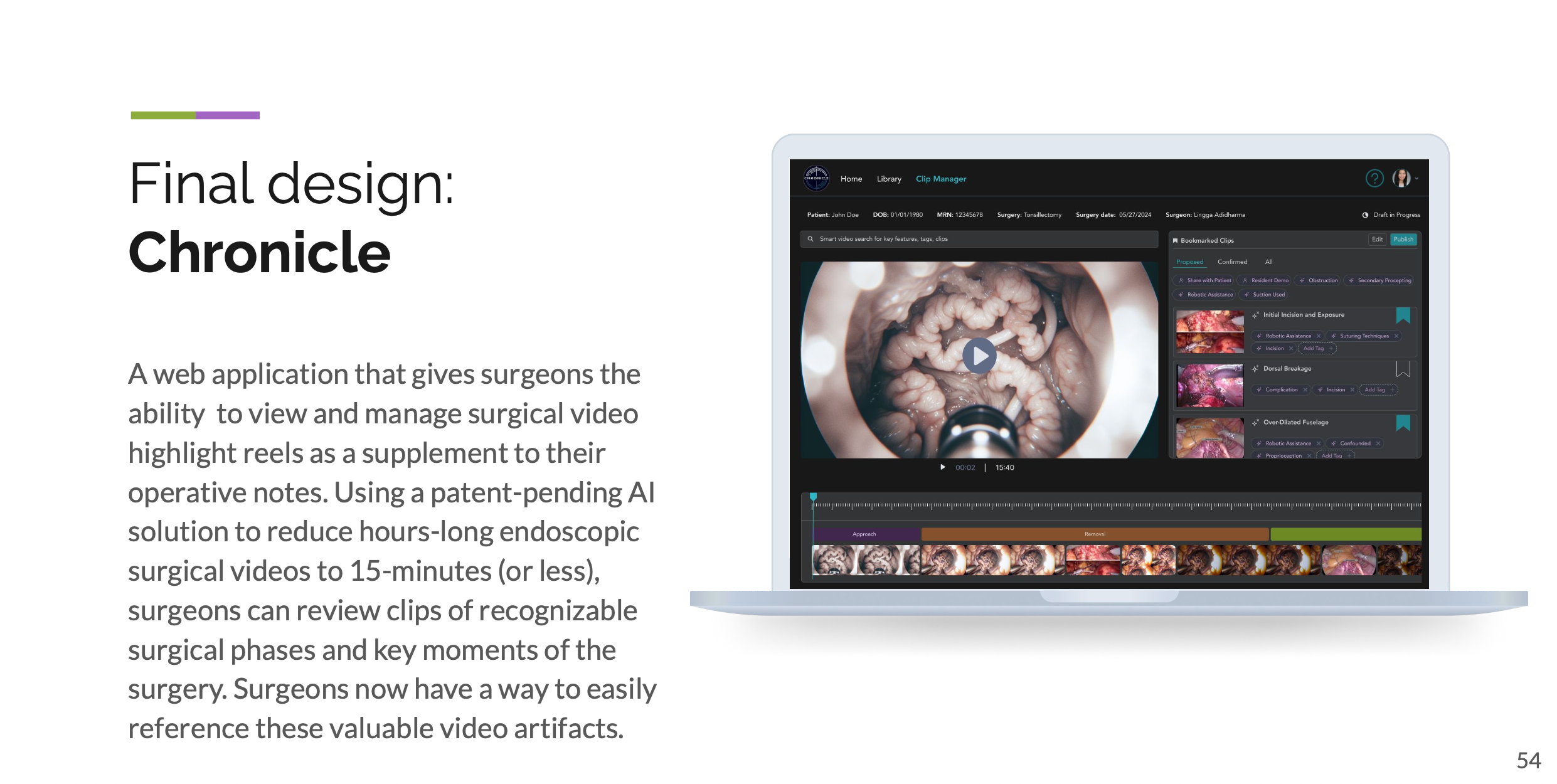




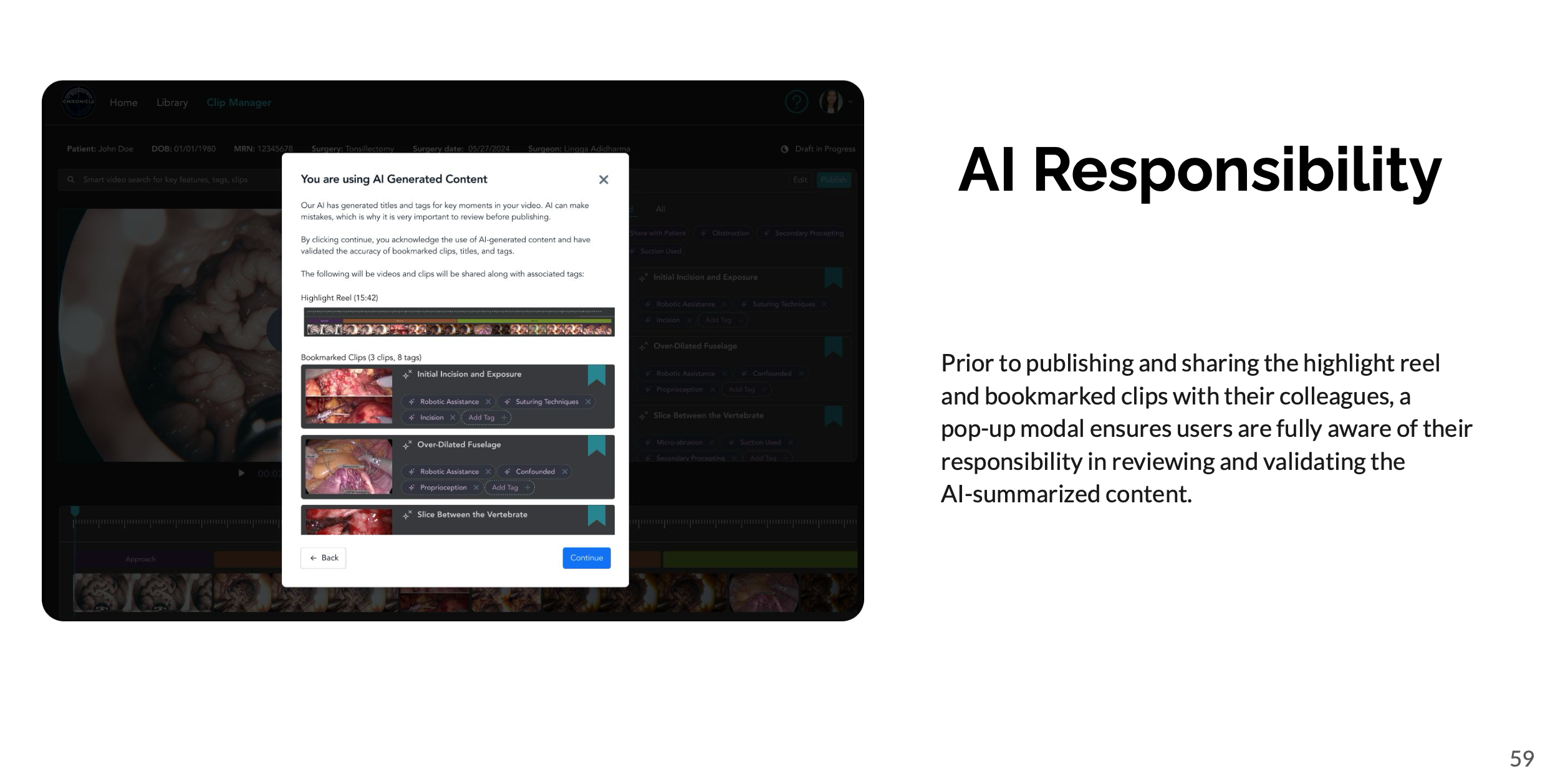
Caption: Final design package showing the product’s core interactions, visual patterns, and accessibility considerations.
With Chronicle, we validated a clear user need and delivered a surgeon-tested concept. Brevity was the next step, expanding research to the broader service ecosystem and exploring multiple models for operational adoption.
Part 2: Brevity – Extending and Scaling the Service
From Capstone to Company
Following the Chronicle capstone, my co-founder and I moved the concept into an operational environment as a startup. We began by handling the logistics of incorporation, equity, and team structure, and brought on our original sponsor, Lingga, as a third co-founder.
While Chronicle had validated that there was a clear user need, we had not yet validated the business case. This became our focus: determining the most viable path for translating the ENT surgical video summarization tool into a sustainable service offering.
Stakeholder engagement expanded to include:
AI developer from the original project team.
Clinical trial coordinator.
Healthcare lawyers specializing in compliance.
UW Institutional Review Board representatives.
Advisors from the UW CoMotion incubator.
These conversations helped us map operational constraints, compliance pathways, and market entry points.
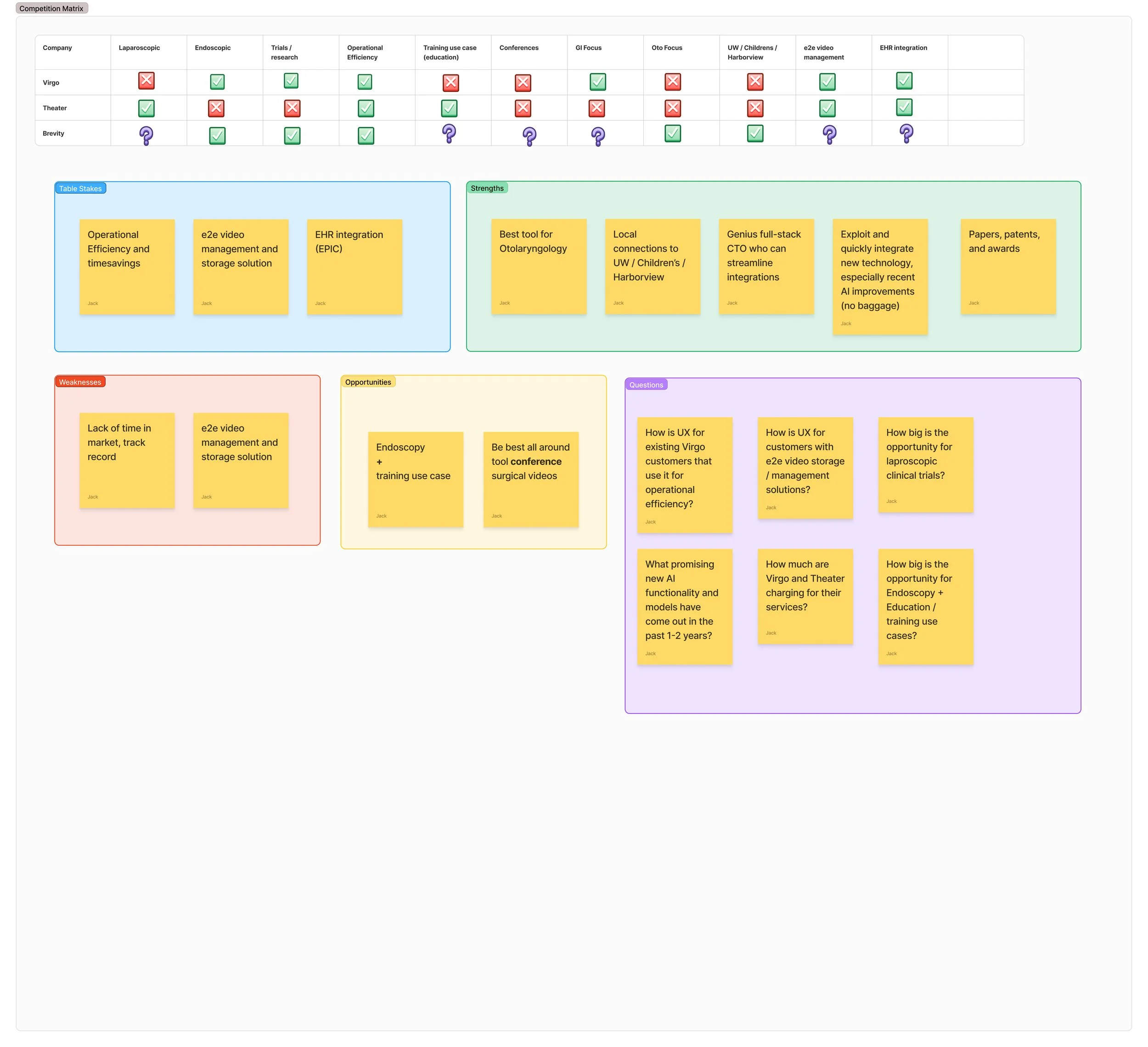
Understanding the Market Context
In parallel with stakeholder interviews, we analyzed the competitive landscape to identify both direct and adjacent services. This included platforms focused on surgical video documentation, AI-powered summarization, EHR integration, and training. The analysis revealed where Brevity could offer differentiated value — particularly in combining physical OR retrieval with secure digital workflows.
Artifact: Competitive Analysis
Caption: Landscape scan of competitor offerings, showing how existing products address documentation, training, and efficiency use cases.
Artifact: Competition Matrix
Caption: Comparative analysis mapping competitors’ features, integrations, and market positioning against Brevity’s potential service footprint.
Exploring Service Opportunities
We ideated around multiple service contexts to test breadth of applicability beyond ENT documentation:
Artifact: Clinical trials use case



Caption: Early explorations of different use cases: clinical trials, conferences, and documentation.
These were not yet validated service designs, but rather a structured way of mapping what we knew, what we needed to learn, and where value might exist.
Pivoting Toward Viable Models
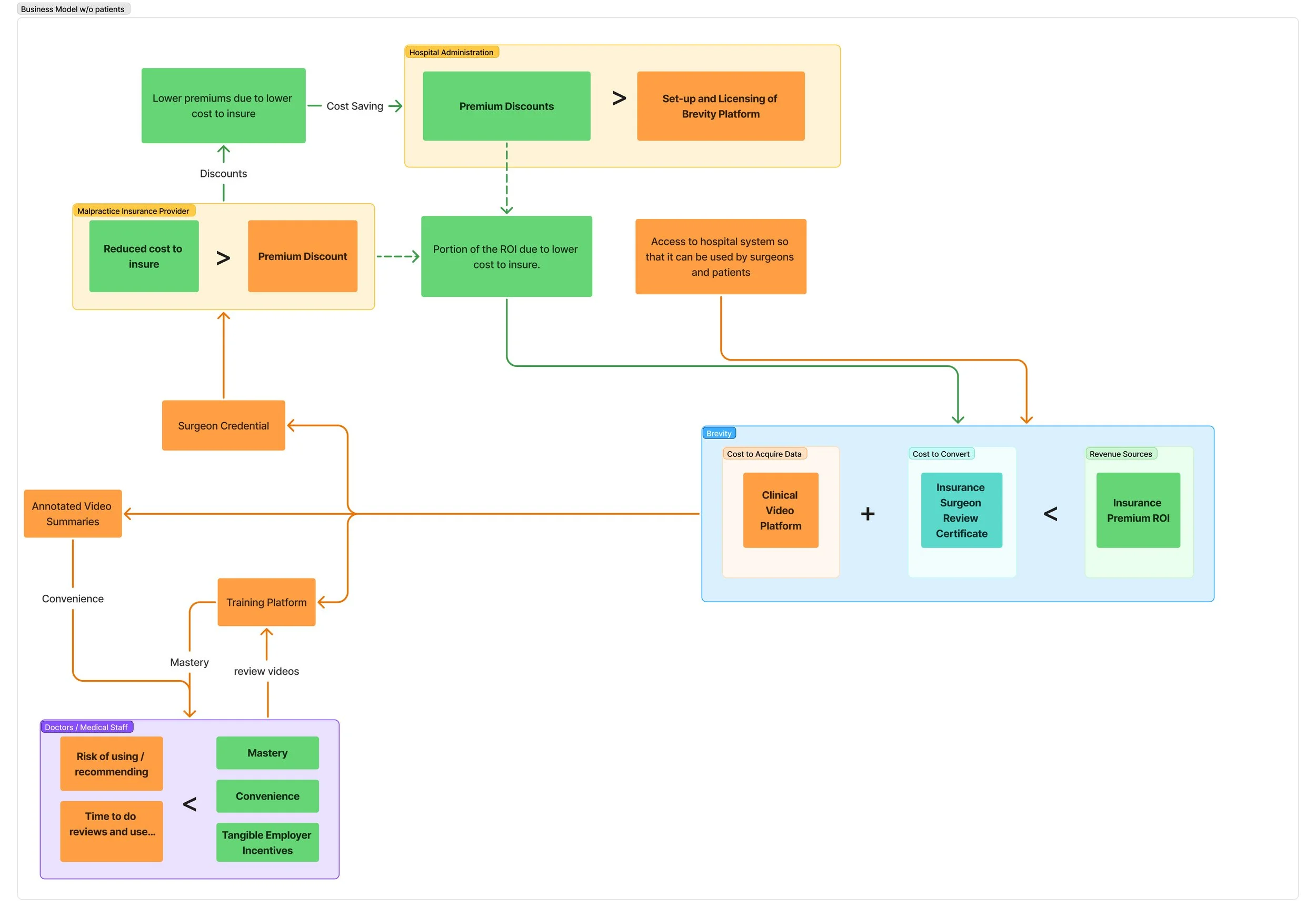
By January, our research indicated that documentation alone had low TAM and weak alignment with hospital purchasing drivers. We explored two alternate models:
Malpractice Risk Reduction – Partnering with insurers to lower premiums in exchange for certified peer-reviewed surgical videos.
Clinical Trial Recruitment – Using video to accelerate patient eligibility review.
We ultimately pursued malpractice reduction due to its larger TAM, though it later failed validation because surgeons resisted peer evaluation and could not commit additional time.
Artifact: Malpractice business model
Caption: Hypothetical service ecosystem mapping revenue and value flows between insurers, hospitals, surgeons, and patients.
Artifact: Malpractice business model without patients
Caption: Alternative service model excluding direct patient-facing components, focusing on insurer–hospital incentives.
Pilot and Service Validation
The final pivot focused on improving consult quality. In a pilot with ENT residents and attendings, residents recorded endoscopic consults, generated AI summaries, and shared them securely for review.
Result: Summarized videos achieved unanimous surgeon confidence ratings of 5/5, compared to significantly lower scores for notes alone.
Quote: “Consult notes alone are essentially useless. Normally, I’d have to scope the patient again. Your videos are significantly better.”
Service Design Considerations Across Phases
Brevity’s offering blended physical and digital elements:
Physical touchpoints: Secure retrieval from OR towers.
Digital workflows: HIPAA-compliant upload, AI processing, review, and storage optimization.
Compliance pathways: IRB oversight, healthcare legal input, and encryption protocols.
Role-based value: Attendings seeking faster decisions, residents needing structured documentation, compliance officers ensuring secure handling.
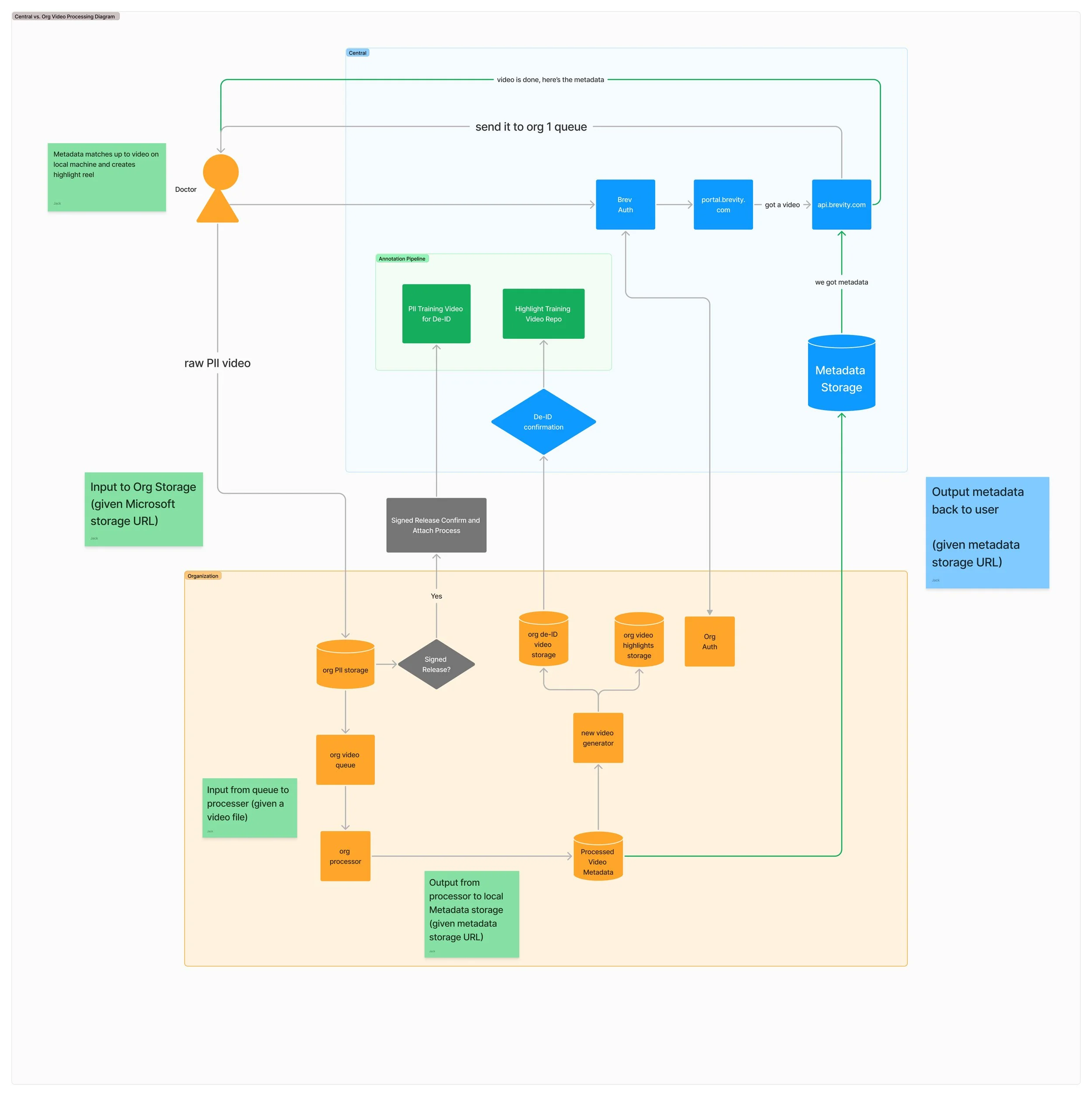
Artifact: User flow
Caption: Updated end-to-end flow showing integration of physical OR retrieval with secure digital processing.
Artifact: Storage optimization
Caption: Backstage workflow for reducing storage costs without compromising compliance.